The Effects of Cranial Electrotherapy Stimulation Therapy Combined with Psychological Intervention in Treating Post-stroke Depression
Wang, X., Xia, P., Lin, Q., Cheng, K., Chen, A., Yang, T., & Xueping, L. I. The effects of cranial electrotherapy stimulation therapy combined with psychological intervention in treating post-stroke depression. Chinese Journal of Physical Medicine and Rehabilitation. 2015; 37(9):680-682.
Funding Source, Location of Study, or Author’s Affiliation
Department of Rehabilitation, Nanjing Hospital Affiliated with Nanjing Medical University, Nanjing, China
Device
Alpha-Stim®
Key Variables
Depression
Objective
To evaluate the effects of cranial electrotherapy stimulation therapy combined with psychological intervention for treating depression alter cerebral infarction.
Design
Eighty (80) patients diagnosed with depression following a cerebral infarction, referred to as Post-Stroke Depression (PSD) were randomly allocated into two groups. Both groups were given routine rehabilitation training and psychological intervention [Treatment As Usual (TAU)], and the experimental group received TAU and Cranial Electrotherapy Stimulation (CES). All patients were evaluated with Hamilton’s depression scale (HAM-D), the mini-mental state examination (MMSE), and the Barthel index (BI) scores before and after four weeks of treatment.
Primary Outcome Measure
- Depression as measured by the Hamilton Depression Rating Scale (HAM-D) which has a maximum score of 52, with 0-7 (no depression); 8-16 (mild depression); 17-23 (moderate depression); and ≥24 (severe depression).
Secondary Outcome Measure
- Cognitive impairment as measured by the Mini-Mental State Examination (MMSE) which has a total score of 30, with 27-30 indicative of normal cognition and a score of <27 indicative of cognitive impairment.
- Activities of daily living (ADLs) as measured by the Barthel index (BI) which has a total score was 100, with >60 indicative of independence (Good with basic self-help ability), 40-60 mildly dependent (Moderate dysfunction needing some help with ADLs, 20-40 suggestive of severe dependency (Clear and obvious dependence on others), and <20 representing total disability (Complete and total dependence on others).
Key Inclusion Criteria
- Clinical diagnosis criteria specified in Classification and Diagnostic Criteria of Mental Disorders in China Edition 3 issued by Chinese Medical Association Psychiatric Society
- First attack of Post-Stroke Depression (PSD)
- Hamilton Depression Scale (HAM-D) ≥18
- Cerebral infarction confirmed by Computed Tomography (CT) or Magnetic Resonance Imagery (MRI)
- Able to cooperate with physical examination and provide informed consent
Key Exclusion Criteria
- Other pre-existing psychiatric disorders, including depression
- Psychoactive drug substances
- Severe systematic illness
- Epilepsy
- Significant cognitive impairment, inclusive of dementia, aphasia, or delirium
Protocol Summary
- Eighty patients diagnosed with depression following a cerebral infarction, referred to as Post-Stroke Depression (PSD) were randomly allocated into two groups. Both groups were given routine rehabilitation training and psychological intervention [Treatment As Usual (TAU)], and the experimental group received TAU and Cranial Electrotherapy Stimulation (CES). All patients were evaluated with Hamilton’s depression scale (HAMD), the mini-mental state examination (MMSE), and the Barthel index (BI) scores before and after four weeks of treatment.
- Control group: The TAU group received psychosocial skills training tailored to the patients’ socioeconomic background and educational level focused on improving face-to-face communication. The medical care team were encouraged to provide a supportive and caring environment to patients. Nursing staff provided easily accessible information regarding the etiology, risk factors, main symptoms, general course of the disease, therapeutic methods and prognosis-related factors, etc. of cerebral infarction. Patients were given opportunities one-on-one aimed at relieving the psychological distress associated with a cerebral infarction, and any confusion, pessimism, or disappointment they may be feeling. With the care team reminding patients of the progress they were making in their recovery and providing words of encouragement. Patients were given the opportunity to have family members join them in the psychosocial skills training they received.
- Experimental group: The active condition received the same psychosocial skills training and supportive environment as the TAU group. In addition, patients received CES using Alpha-Stim for 60 minutes twice daily during the first two weeks, and for 60 minutes daily every two days for the remaining two weeks.
Device Application Protocol
Alpha-Stim CES was administered in a supine position at 0.5 Hz and 10-500 μA for 60 minutes. A standard course of treatment was four weeks. In the first two weeks, CES was given twice a day for 60 minutes; and in the second two weeks once every two days for 60 minutes.
Statistical Analysis Plan
SPSS 17.0 statistical software package was used for data processing. The measurement data were compared through t-test, and the enumeration data were compared through χ2 test, with p<0.05 indicating a statistically significant difference.
Mood
- The comparison of the therapeutic effect of TAU in comparison to TAU+CES on depression symptoms was analyzed by comparing pre and post HAM-D scores.
- The reduction rate of HAM-D scores before and after treatment was taken as the evaluation criteria.
- A reduction rate of HAM-D score = [(HAM-D score before treatment -HAM-D score after treatment)/HAM-D score before treatment] x 100%, in which ≥75% indicated Cured, ≥50% Markedly Effective, ≥25% Effective, and <25% Ineffective.
Cognition
- Variations in the MMSE score pre and post-treatment across the two groups were used to evaluate any changes to cognitive impairment.
Independence
- The BI score was used to evaluate changes to the number of ADLs that patients were able to do before and after treatment.
Results
Subjects
- A total of 80 patients were randomly assigned to the control group (TAU) and the experimental group (TAU+CES), with 40 patients in each group. There was no statistically significant difference between the two groups in terms of gender, average age, level of education, average course of the disease, and other general data, etc. (p>0.05) were comparable.
- In the treatment group (TAU+CES), there were 19 males and 21 females aged between 40-82 years old, with mean (SD) age of 56.63±9.71 years and mean (SD) of 10.44±2.72 years of education, and a mean (SD) course of disease of 2.93±1.69 months. In the experimental group, 18 cases were diagnosed with left hemiplegia and 22 cases with right hemiplegia.
- In the control group (TAU), 17 males and 23 females were enrolled, aged between 39-82 years, with a mean (SD) age of 57.15±9.75 years, mean (SD) education 10.26±2.41 years, and mean (SD) course of disease of 2.94±1.37 months. In the control condition, 24 cases of left hemiplegia and 16 cases of right hemiplegia were enrolled.
Data Analysis
Before treatment, the differences in HAM-D, MMSE, and BI scores between the two groups were not statistically significant (p>0.05). After 4 weeks of treatment, HAM-D, MMSE, and BI scores of both groups were improved in comparison to those before treatment. The reduction in depression, improved cognition, and greater independence as evidenced by HAM-D, MMSE, and BI scores in the TAU+CES group showed were superior to those in the control group, with statistically significant difference (p<0.05).
During treatment, no adverse reactions were found in the two groups. After four weeks of treatment, the total marked effective rate of treatment was higher in the CES+TAU group than the TAU group (p<0.05).
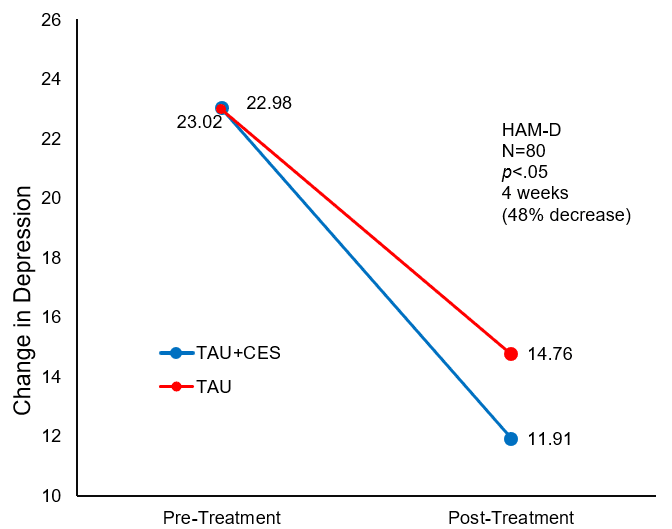
Change in mean HAM-D Score pre and post-treatment for the control (TAU) and experimental (TAU+CES) condition
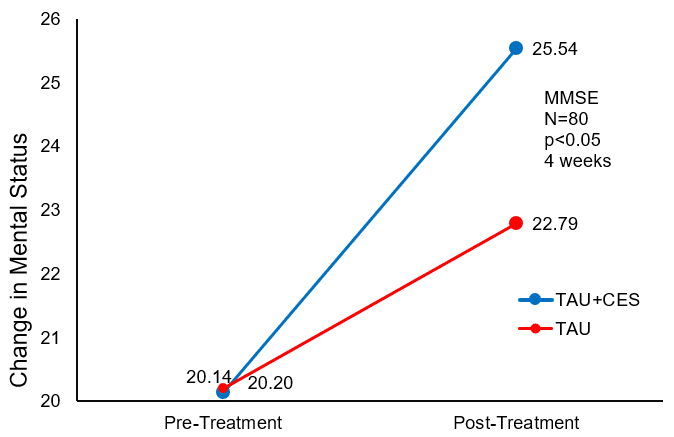
Change in mean MMSE Score pre and post-treatment for the control (TAU) and experimental (TAU+CES) condition.
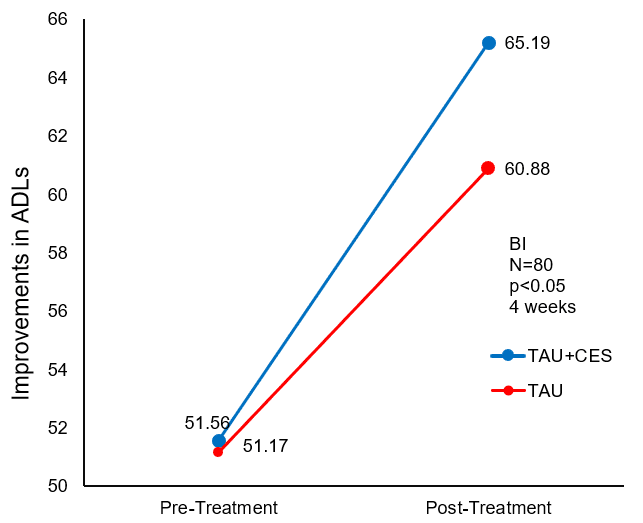
Change in mean BI Score pre and post-treatment.
Conclusion
There was no significant difference between the two groups in terms of any of the measures before treatment. After four weeks of treatment, both groups had improved significantly, but the improvements on all measures were significantly better in the treatment group. CES combined with psychosocial skills training significantly reduced symptoms of depression and increased cognitive function in patients with PSD, resulting in significant improvements to the patients’ independence and ADL. The authors conclude that CES stimulates the release of endorphins, in addition to stimulation the release and reabsorption of dopamine, concurrently addressing any imbalance between the adrenergic and cholinergic.
Limitations
While this study was a randomized controlled trial, it was not double-blind. Therefore, both participants and investigators were aware of assigned intervention category. Additionally, the authors do not mention their procedures for missing data. According to the Cochrane risk-of-bias tool, each of these conditions can introduce unintended bias into a study.
Study Quality: FAIR

