Clinical Efficacy of Assisted Cranial Electrotherapy Stimulation Treatment on Depression
Wei Y., Yang Z., Pan H., Zhao S-J., Fang J-Z. Clinical Efficacy of Assisted Cranial Electrotherapy Stimulation Treatment on Depression. Neural Injury and Functional Reconstruction. July 2014, 9(4):317.
Funding Source, Location of Study, or Author’s Affiliation
Department of Psychiatry, The Third People’s Hospital of Changshu City, Jiangsu 215500, China
Device
Alpha-Stim®
Key Variables
Depression and anxiety.
Objective
To observe the curative effect and safety of antidepressants combined with cranial electrotherapy stimulation (CES) in treatment for depression patients
Design
A group of patients diagnosed with depression and anxiety were randomly allocated into two groups. The control group received antidepressant medication, and the experimental group CES. The treatment cycle for both groups was 6 weeks. Pre- and post-treatment depression scores were measured using the Hamilton Depression Rating Scale (HAM-D) and anxiety using the Hamilton Anxiety Rating Scale (HAM-A). The level of cognitive impairment was assessed using the Wisconsin Card Sorting Test (WCST). With the safety of the treatment modalities assed using the Treatment Emergent Symptom Scale (TESS).
Primary Outcome Measure
Pre and post scores for:
- Depression measured by Hamilton Depression Rating Scale (HAM-D)
- Anxiety assessed by the Hamilton Anxiety Rating Scale (HAM-A)
Secondary Outcome Measure
- Cognition as measured by the Wisconsin Card Sorting Test (WCST)
- Safety as assessed by Treatment Emergent Symptom Scale (TESS)
Key Inclusion Criteria
- Diagnosis of depression following the Classification and Diagnostic Criteria of Mental Disorders in China Edition 3 (CCMD-3)
- HAM-D ≥17
- Male or female aged 16-68 years old
Key Exclusion Criteria
- Prior diagnosis of a neurodegenerative disease
- History of or current substance use or dependence
- Pregnant, lactating, or planning to become pregnant
- Diagnosis of epilepsy
- Implanted medical devices, including pacemakers, insulin pumps
Protocol Summary
- A total of 80 patients were randomly allocated into two groups of 40. Both groups received Treatment as Usual (TAU) consisting of antidepressant medication, with the experimental group receiving CES using Alpha-Stim in addition to medication (TAU+CES).
- The drug classes for the antidepressant medication included Noradrenergic and Specific Serotonergic Antidepressants (NaSSA), Selective Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), Selective Serotonin Reuptake Inhibitor (SSRIs), Serotonin Antagonist and Reuptake Inhibitors (SARIs), and Tricyclic Antidepressants (TCAs).
| Drug Class | Condition & Frequency | |
| TAU+CES | TAU | |
| Noradrenergic and Specific Serotonergic Antidepressants (NaSSA) | 14 | 14 |
| Selective Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) | 12 | 13 |
| Selective Serotonin Reuptake Inhibitor (SSRIs) | 9 | 7 |
| Serotonin Antagonist and Reuptake Inhibitors (SARIs) | 3 | 3 |
| Tricyclic Antidepressants (TCAs) | 2 | 3 |
| Total | 40 | 40 |
The number of patients in each drug class.
- During the CES treatment cycles, combination with other medications or treatments was not permitted (i.e., antipsychotics, antidepressants, mood stabilizers, electric convulsive therapy, or systematic psychotherapy).
- CES therapy was administered using Alpha-Stim as per the manufacturer’s instructions. Subjects received four courses of treatment, each treatment cycle lasting 20 minutes, over five days, with a two-day rest period between treatment cycles, resulting in 20 days of treatment over six weeks.
- The symptom severity and adverse drug reactions were evaluated respectively at the time of admission and the end of 1, 2, 4, and 6 weeks of treatment, and patients’ cognitive functions were evaluated at the time of admission and the end of the 6th week.
- Treatment response was assessed by two attending psychiatrists who had been rigorously trained, respectively evaluated the individuals in the two groups and tested their consistency on their scale evaluations (Kappa=0.86).
Device Application Protocol
Patients were instructed to (1) clean their earlobes with a wet cotton pad, (2) apply the conductive solution, and (3) gently clamp the electrodes around the base of their earlobes. Patients were advised to relax and lay down in a location where they would not be disturbed. Instructions to set the Alpha-Stim CES device to a frequency of 0.5 Hz and intensity between 10-500 μA were given to patients. Each patient had the ability to self-calibrated the minimum threshold of intensity by gradually increasing it until they experienced a mild tingling sensation. The course of treatment was 20-minutes over a five-day period. Each course was started two days after completion of the former one, and each patient received four courses of treatment, 20 treatments in total.
Statistical Analysis Plan
- The reduction of HAM-D scores was used as the evaluation indicator of efficacy (i.e., HAM-D score ≤7 indicating clinical recovery, and HAM-D reduction ≥50% indicating effectiveness).
- Significance testing using t-tests, chi-square, and repeated measures Analysis of Variance (ANOVA) at a statistically significant level of p<0.05.
- SPSS 17.0 statistical software was used to analyze the data.
Results
Subjects
- The TAU+CES condition included 40 patients, 15 males, and 25 females, with a mean (SD) age of 36.36±13.53 years, and a depression diagnosis with a mean (SD) of 18.74±16.25 weeks; with six patients having a family history of depression. The mean (SD) total HAM-D score at baseline was 25.32±5.24.
- The TAU group included 12 males and 28 females, a total of 40 subjects with a mean (SD) age of 34.72±12.48 years, and a diagnosis of depression of with a mean (SD) of 71±15.52 weeks; of which seven subjects reported a family history of depression. The mean (SD) total HAM-D score at baseline was 25.89±4.67.
- The dose of each antidepressant drug was adjusted to the therapeutic dose within 1-2 weeks according to individual tolerance. The difference in type, composition and mean dose of antidepressant drugs between the two groups was not significant (p>0.05).
- No significant differences between groups in cognitive impairment as measured by WCST scores were reported at baseline.
- No significant changes in hemogram, ECG, liver, and kidney functions were found between the two groups.
- A total of five patients across the two groups did not complete or were withdrawn from the study. The difference in withdrawal rate between the two groups was not statistically significant (x2=0.213, p>0.05).
Data Analysis
After the treatment the HAM-D and HAM-A scores in the two groups were significantly lower than before treatment (p<0.01). In the sixth week, the assisted efficiency and curative rates between the two groups showed no significant difference (p>0.05). In the 4th week, the efficiency in the TAU+CES group was significantly higher than in TAU group (p< 0.05).
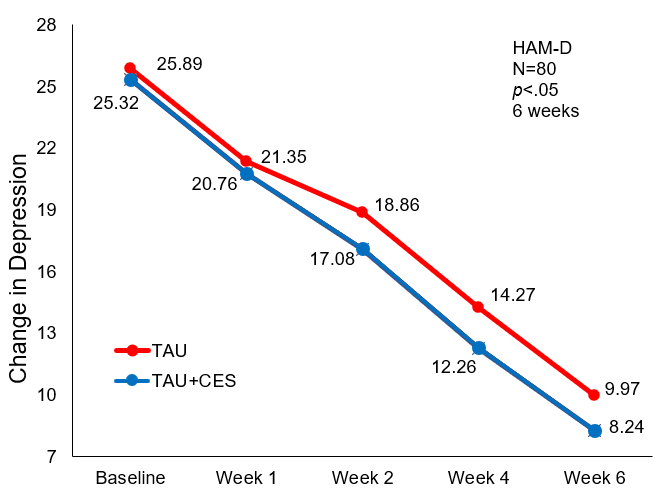
Mean HAM-D Score Baseline Through Week 6 of Treatment
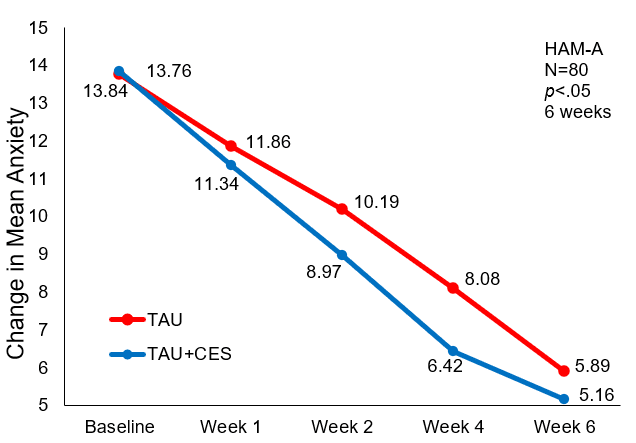
Mean HAM-A Score at Baseline Through Week 6 of Treatment.
Efficacy: The efficacy of treatment was assessed at Weeks 2, 4, and 6, and shown in the table below. The efficacy and curability rate of the TAU+CES condition was significantly higher (p<0.05) at the 4th week of treatment than the TAU condition. No significant difference in efficacy or curability between the two conditions was observed at the 2nd or 6th week post-treatment.
| Group | N | Week 2 | Week 4 | Week 6 | |||
| Effective | Cured | Effective | Cured | Effective | Cured | ||
| TAU | 37 | 6(16.22%) | 1(2.70%) | 11(29.73%) | 6(16.22%) | 26(70.27%) | 18(48.65%) |
| TAU+CES | 38 | 11(28.95%) | 2(5.26%) | 20(52.63%) | 10(26.32%) | 30(78.95%) | 21(55.26%) |
| x2 | 1.73 | 0.32 | 4.06 | 1.14 | 0.75 | 0.33 | |
| P | 0.188 | 0.572 | 0.044 | 0.286 | 0.388 | 0.566 | |
Comparison of efficacy and curability
Response: At baseline, there was so significant difference in HAM-D (p>0.05) between the two groups. The TAU comparator and the TAU+CES condition both resulted in a reduction in depression and anxiety symptoms as evidenced by the lower HAM-D and HAM-A scores (p<0.01). Symptoms of disordered sleep and depression (total HAM-D) were significantly lower at the end of the 2nd week of treatment in the TAU+CES condition compared to the TAU group. Significant reductions in symptoms of depression, anxiety, and occurrence of disordered sleep were reported in the TAU+CES group at the end of the 4th week of treatment. These improvements in symptoms are evidenced by the lower total HAM-D (p<0.05); HAM-A, retardation, and frequency of disrupted sleep (p<0.01). In addition, faster treatment response times were shown in the TAU+CES condition.
Cognition: After six weeks of treatment, the TAU and the TAU+CES groups showed significant improvement in cognitive impairment (p<0.05 and p<0.01). With a greater number of correct responses and a lower number of incorrect responses from baseline to post-treatment in the TAU+CES group than that in the TAU group (p<0.05). The occurrence of random incorrect and classified responses increased from baseline to six weeks post-treatment in both groups, but there were no significant differences between the groups.
Risk: In the TAU+CES group a total of 38 patients completed the study and two were withdrawn (one self-discontinued medication and one switched from depression to mania). While in the TAU condition 37 patients completed the study and three were withdrawn (one switching from depression to mania, one requiring mild electroconvulsive therapy (mECT), and one self-discontinuing medication). The difference in withdrawal rate between the two groups was not statistically significant (x2=0.213, p>0.05). The majority of minor adverse reactions or side effects occurred within the first two weeks of treatment. As treatment progressed, side-effects diminished and were well tolerated. There was no significant difference in the TSSS score between the TAU and TAU+CES groups, with details shown in the table below. The comparison of the adverse events between the two groups revealed no difference (p >0.05). The reported adverse events are known side-effects of antidepressant medication and unrelated to Alpha-Stim use.
Conclusion
In this study, TAU and TAU+CES effectively reduced symptoms of depression, anxiety, and disordered sleep, with higher treatment response rates in the TAU+CES condition at 4 weeks post-treatment (p<0.05). Cognitive decline associated with depression showed a greater improvement in the TAU+CES group.
The authors concluded that CES was an effective augmentation strategy to pharmacological treatment. The TAU+CES condition increased the speed of treatment response and efficacy. Additionally, CES is a safe treatment approach with minimal and self-limiting side effects. The authors describe a mechanism of action for CES where the electrical stimulation reaches the thalamus, hypothalamus, brainstem, and limbic and reticular system resulting in greater brain electrical activity mapping (BEAM) and the release of 5-hydroxytryptamine (5-HT), endorphin, and melatonin. With a commensurate increase in the concentration of γ-aminobutyric acid (GABA), which collectively quickly and effectively relieves depression, anxiety, and disordered sleep, in addition to cognitive impairment associated with depression.
Limitations
This was a well-designed, randomized controlled study, but it was not a double-blind study. Therefore, limitations include both participants and investigators being aware of assigned interventions. The researchers do not discuss their procedures for missing data. According to the Cochrane risk-of-bias tool, each of these conditions may introduce unintended bias into a study.
Study Quality: FAIR

