Acupuncture combined with cranial electrotherapy stimulation on generalized anxiety disorder: A randomized controlled trial
Liu, E., Zhang, W., Wang, J., Zhao, F., & Bai, Y. Acupuncture combined with cranial electrotherapy stimulation on generalized anxiety disorder: A randomized controlled trial. Chinese Acupuncture & Moxibustion. 2020; 40(11).
Funding Source, Location of Study or Author’s Affiliation
Department of TCM, First Hospital of Hebei Medical University, Shijiazhuang, China
Device
Alpha-Stim® SCS
Key Variables
Anxiety and Quality of Life.
Objective
To observe the therapeutic effect of acupuncture combined with cranial electrotherapy stimulation (CES) on generalized anxiety disorder (GAD).
Design
A randomized controlled study comparing the effectiveness of four (K=4) different treatment groups (1) medication only (MED), (2) acupuncture only (ACU), (3) cranial electrotherapy stimulation only (CES), and (4) acupuncture plus CES (ACU + CES) for the treatment of generalized anxiety disorder (GAD). The medication only (MED) group was considered the control group as it received treatment-as-usual (TAU), and the acupuncture only (ACU) and CES only (CES) and acupuncture plus CES (ACU+CES) are the experimental groups.
Baseline and post-treatment anxiety scores were measured using the Hamilton Anxiety Rating (HAM-A) scale. Similarly, baseline and end of treatment quality of life were assessed using the World Health Organization Quality of Life Questionnaire-Brief Version (WHOQOL-BREF). Adverse events were measured using the Treatment Emergent Symptom Scale (TESS). Patients were assessed at the end of the study and relapse rates reassessed 12 months after the end of treatment.
Primary Outcome Measure
- Anxiety
- Assessed using the Hamilton Anxiety Rating Scale (HAM-A).
- The HAM-A includes a severity scale for each item from 0 “Not present” to 4 “Severe”
- Scores range from 0–56 with <17 indicating “Mild severity”; 18–24 “Mild to moderate severity”, and 25–30 “Moderate to severe”.
- Quality of Life
- Measured by the World Health Organization’s Quality of Life Questionnaire Brief Version (WHOQOL-BREF)
- The WHOQOL-BREF is a 26-item instrument consisting of four domains: physical health (7 items), psychological health (6 items), social relationships (3 items), and environmental health (8 items), and other general health items.
- Each item in the WHOQOL-BREF is scored from 1 to 5 on a response scale.
Secondary Outcome Measure
- Side Effects
- Measured by the Treatment Emergent Symptom Scale (TESS).
- The TESS scale is used to assess adverse events that first occurred or worsened in severity after initiation of treatment or therapy.
- The scale includes measures of behavioral toxicity, laboratory abnormalities, cardiovascular, autonomic, and nervous system reactions, body weight, headache, and appetite changes.
- Scores range from 0 to 4, with a higher score indicative of more serious adverse reactions.
Key Inclusion Criteria
- Met criteria for Generalized Anxiety Disorder (GAD) according to the Chinese Classification of Mental Disorder, 3rd edition (CCMD-3). The clinical manifestations of GAD include restlessness, insomnia, a sense of dread, feeling constantly “on edge”, dizziness, irritability, difficulty concentrating, and muscular tension or pain.
- Diagnosis of GAD ≥6 months
- Hamilton Anxiety Rating (HAM-A) scale ≥14
- Age <80 years
- Provide informed consent
- Be willing to be randomized into one of the treatment groups
- Follow the study protocol
Key Exclusion Criteria
- Chronic medical conditions such as severe heart, brain, liver, kidney, hematopoietic system, etc.
- Not a good candidate or unfit for CES or acupuncture treatment.
- Use of anxiolytic medication in the last two weeks or discontinued medication within the last two weeks.
- Other psychiatric disorders.
Protocol Summary
Patients in all four groups (K=4) received treatment for sixty (60) days irrespective of group assignment.
- Medication only (MED): in the medication (MED) only TAU group patients were treated with oral tandospirone citrate (brand name Sediel) an anxiolytic and antidepressant drug used in China and Japan. The dosage was 10mg after breakfast, lunch, and dinner.
- CES only (CES): the CES only (CES) group received treatment using the Alpha-Stim® SCS device daily for 60 minutes each time.
- Acupuncture only (ACU): the acupuncture only (ACU) group received traditional acupuncture applied daily for 30 minutes to (1) Baihui (GV 20), (2) Sishencong (EX-HN 1), (3) Yintang (GV 29),(4) Shenting (GV 24), etc.
- Acupuncture plus CES (ACU+CES): the acupuncture plus CES (ACU+CES) group received CES treatment before acupuncture. The treatment protocol for the acupuncture and CES were the same as the acupuncture only (ACU) and CES only (CES) group.
Device Application Protocol
CES was administered using the Alpha-Stim® SCS, and patients were instructed to lay supine or sit comfortably, saturate the electrode pad with conducting liquid, then clamp the electrode at the base of both earlobes. Once the device was attached patients were instructed to turn the power switch on and adjust the intensity from level 0-5 until a slight feeling of dizziness or a sensation of tingling on the earlobes occurred. Treatment was daily, for 60 minutes each time, for 60 continuous days of the treatment trial.
Statistical Analysis Plan
Changes in HAM-A and WHOQOL were observed, the clinical effect was evaluated, and the anxiety relapse rate was measured in all four groups at follow-up one year after treatment ended. The relapse rate was set at a HAM-A score ≥14.
The therapeutic effect was evaluated by comparing the change in HAM-A scores. HAMA score indicator = [(HAM-A score before treatment – HAM-A score after treatment)/HAM-A score before treatment] ×100%. The results were interpreted as HAM-A score (1) ≥75% “Cured”, (2) 50%≤ HAM-A score indicator <75% “Excellent”, (3) 25%≤ HAM-A score indicator <50% “Effective”, (4) <25% HAM-A score indicator “Ineffective”.
SPSS 18.0 software was used for statistical analysis, and the measurement data were described by mean ± standard deviation (SD). The comparison among groups is used with single-factor analysis of variance (ANOVA), and the comparison between two groups is checked by Least Significant Difference (LSD); the enumeration data is checked by χ2. A significance level of p<.05 is used to determine a statistically significant difference.
Results
Subjects
A total of 200 patients with GAD were randomly allocated into four groups (K=4) using a random number table, with 50 cases per group (n=50). Comparison of subjects’ general characteristics at baseline across all groups, including gender, age, and course of the disease were not statistically significant (p>.05). The groups can be considered comparable.
The MED only (MED) group included 22 males and 28 females, aged 27-70 years, representing a mean age 38±3 years, and a course of disease between 6-40 months, equating to a mean course of 13.6±2.6 months.
In the CES only (CES) group 22 males and 28 females aged 25-69 years were enrolled, with a mean age of 37±3 years, and a course of disease between 7-39 months, reflecting a mean of 13.0±3.1 months since disease onset.
The acupuncture only (ACU) group enrolled 20 males and 30 females, aged 25-71 years, reflecting a mean age of 38±3 years, and a course of disease ranging from 6-41 months, with a mean onset of 14.0±2.4 months.
The acupuncture plus CES group (ACU+CES) enrolled 21 males and 29 females aged from 27-72 years old and having a mean age of 38±2 years, and a disease course of 7-42 months, and a mean of 13.5±2.7 months since onset.
Data Analysis
Across all four groups, patients reported benefitting from the treatment they received. The level of anxiety was significantly reduced as evidenced by the lower HAM-A scores (p<.05). Furthermore, quality of life as measured by the WHOQOL- BREF significantly improved following treatment as indicated by the higher scores post-treatment (p<.05).
Anxiety:
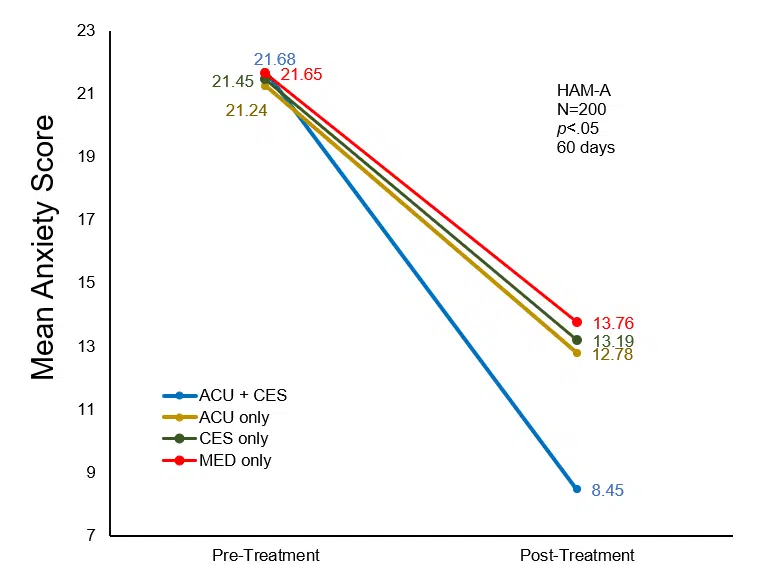
No statistically significant difference in the level of anxiety between the four groups was reported before treatment (p>.05). Following treatment, the HAM-A score of all four groups decreased significantly (p<.05). The acupuncture plus CES (ACU+CES) group reported the largest decrease in anxiety from baseline to post-treatment (p<.05).
Comparison of anxiety (HAM-A) score before and after treatment in each group.
| Group | Cases | Before treatment | After treatment | Before treatment – after treatment |
| ACU+CES | 50 | 21.68±2.13 | 8.45±1.211 | 13.12±1.782,3,4 |
| ACU only | 50 | 21.24±2.17 | 12.78±1.671 | 8.73±1.21 |
| CES only | 50 | 21.45±2.05 | 13.19±1.431 | 7.89±1.13 |
| MED only | 50 | 21.65±2.13 | 13.76±1.681 | 6.56±0.76 |
Note: Through comparison with that before treatment of this group 1p<.05; through comparison of difference before and after therapy of acupuncture only group (ACC) 2p<.05; through comparison of difference before and after therapy of CES only group (CES) 3p<.05; through comparison of difference before and after therapy of medication only group (MED) 4p<.05.
Comparison of anxiety (HAM-A) score before and after treatment in each group.
Note: acupuncture plus CES (ACU+CES); acupuncture only (ACU); CES only (CES); medication only (MED).
Quality of Life:
At baseline, no statistically significant difference in the quality of life as measured by the WHOQOL-BREF was reported between the four groups (p>.05). After therapy, the WHOQOL-BREF score of all four groups of patients increased significantly (p<.05). The patients in the acupuncture plus CES (ACU+CES) group reported a larger increase in WHOQOL-BREF scores than the other three groups (p<.05). The increase in scores reflects greater quality of life post-treatment.
Comparison of WHOQOL-BREF score before and after therapy in each group
| Group | Cases | Before therapy | After therapy | After therapy – before therapy |
| ACU+CES | 50 | 65.12±4.21 | 80.32±3.671 | 15.37±2.022,3,4 |
| ACU only | 50 | 65.28±3.89 | 74.76±3.891 | 9.12±1.23 |
| CES only | 50 | 65.02±4.17 | 74.13±4.231 | 8.96±1.18 |
| MED only | 50 | 64.76±4.24 | 73.98±4.141 | 8.72±1.10 |
Note: Through comparison with that before therapy of acupuncture plus CES (ACC+CES) group 1p<.05; through comparison of difference before and after treatment of acupuncture only group (ACU) 2p<.05; through comparison of difference before and after treatment of CES only (CES) group 3p<.05; through comparison of difference before and after treatment of medication only (MED) group 4p<.05.
Adverse Events:
A comparison of adverse events across the four groups as measured by the TESS scores indicates that patients in the medication only (MED) group reported significantly higher side effects than the other treatment conditions (p<.05). In addition, the relapse rate at follow-up, 1-year post-treatment was significantly higher in the medication only (MED) group than those of the other three groups (p<.05).
Comparison of TESS score and follow-up relapse rate after treatment in each group
| Group | Cases | TESS score | Relapse | |
| Cases | Relapse rate/% | |||
| ACU+CES | 50 | 0.17±0.281 | 2 | 4.01 |
| ACU | 50 | 0.13±0.311 | 6 | 12.01 |
| CES only | 50 | 0.15±0.241 | 5 | 10.01 |
| MED only | 50 | 1.04±0.68 | 17 | 34.0 |
Note: acupuncture plus CES (ACC+CES); acupuncture only (ACU); CES only (CES); medication only (MED);
through comparison with medication group 1p<.05.
Effectiveness:
The total effective rate of the medication only (MED) group was 80%, for the CES only group (CES) 80%, and for the acupuncture only (ACU) group 84%. Although the improvements to patients’ life following treatment are substantial, all the treatment conditions were significantly lower than the 96% effective rate reported by the acupuncture plus CES group (ACU+CES) (p<.05).
Comparison of clinical effect of each treatment group
| Group | Case | Cured | Excellent | Effective | Ineffective | Total effective rate/% |
| ACU+CES | 50 | 11 | 25 | 12 | 2 | 96.0 |
| ACU only | 50 | 6 | 19 | 17 | 8 | 84.01 |
| CES only | 50 | 6 | 15 | 19 | 10 | 80.01 |
| MED only | 50 | 4 | 13 | 23 | 10 | 80.01 |
Note: acupuncture only (ACU); CES only (CES); medication only (MED); acupuncture plus CES (ACU+CES);
through comparison with acupuncture plus CES group (ACU+CES) 1p<.05.
Conclusion
Overall, the total effective rate in the acupuncture plus CES group was significantly better than the other three groups (p<.05). Noticeably, the reduction in anxiety and improvements to the quality of life reported by patients in the acupuncture plus CES (ACU+CES) group was significantly greater than the other three groups (p<.05).
The authors conclude acupuncture combined with CES can effectively relieve symptoms in patients with GAD, improve their quality of life, reduce the occurrence of adverse reactions, and the relapse rate. The authors support the mechanism of action proposed in the literature that CES therapy stimulates the secretion and release of a range of neurotransmitters including 5-hydroxytryptamine and endogenous morphine peptides by the cerebral cortex and hypothalamus, that subsequently support the reduction of anxiety symptoms. In this study, the CES group and the MED group had similar reductions in anxiety symptoms and improvements in quality of life. However, the CES group experienced significantly fewer and less severe side effects than the medication group. Additionally, the rates of relapse were over three times more in the medication group than in the CES at one-year follow-up. Thus, the clinical effectiveness of CES is superior to that of medication.
Limitations: This was a strong RCT with one-year follow up that measured both anxiety and quality of life. However, the randomization was not blinded and both participants and investigators were aware of group assignments. Additionally, the authors did not discuss an a priori plan for missing data in this article.
Study Quality: GOOD